Masivukeni
HIV Treatment Adherence Intervention for Clinical Use In South Africa
Project Dates: 2009-2010
Partners: Columbia University Center for New Media Teaching & Learning (CCNMTL), HIV Center for Clinical and Behavioral Studies , University of Cape Town, National Institute of Mental Health
My Roles: Intervention and Activity Design, Cross-Cultural Research, Interaction Design
In 2009, patients' inability to adhere to unforgiving HIV treatment protocols was a major problem in South Africa, often leading to drug resistance and death.
The 2007 UNAIDS report estimated that 18.5% of South Africa's adult population were living with HIV/AIDS; a larger infection rate than in any other single country in the world. Yet in that same year, only 28% of people in South Africa with advanced HIV/AIDS were receiving anti-retroviral treatment (ART).
In contrast to the United States, where a variety of treatment options were available and becoming increasingly easier for patients to take effectively, in South Africa, only two sets of drugs were available, both requiring near-perfect adherence to maintain efficacy and avoid drug resistance. Missing a single dose of medication by as little as an hour could render a previously perfect medication record meaningless. Once patients had developed resistance to both sets of drugs, they were essentially out of options.
This was an especially wicked problem for a variety of reasons. Drugs had to be taken twice per day, at exactly the same time. Many people had kept their HIV status secret and therefore were alone in remembering — and finding a way — to take their pills on time. Medications often had major side effects, making them difficult to tolerate. Clinics were crowded and far away, requiring patients to face seemingly impossible obstacles of scheduling, transportation, and childcare in order to get prescriptions filled. Stigma, denialism, and a belief that local healers were more effective than Western medicine remained major problems.
Masivukeni, which translates to 'Let's wake up!' in the Xhosa language, is a computer-assisted program designed to support lay counselors at health clinics in South Africa in assisting HIV-positive adults with effective adherence to their anti-retroviral drug regimens.
The program uses enhanced text, imagery, animations, audio, and video to teach the basics of how HIV and anti-retrovirals affect health and to build problem solving and social support skills that patients use to overcome barriers to treatment adherence.
In designing Masivukeni, we collaborated closely with research partners, community stakeholders, and potential users from Cape Town on design, language, and activities to ensure that the program was culturally relevant and effective. As such, Masivukeni follows South Africa's "buddy system" for new patients beginning anti-retroviral treatment, in which a patient is asked to find a support partner who can attend counseling with them before the first drugs are dispensed.
Introductory Video
Pill Regimen Activity | Early Wireframe
One very important element of Masivukeni was simply practical information and reminders. The simple action of moving appropriate pills to cups representing a dosage time — and thinking about what taking the pills at that time meant in physical reality — was very helpful for patients both in setting up correct understanding of their personalized regimen and in establishing sustainable medication plans. At the end of this activity, patients could choose to print this screen to take away as a helpful daily reminder of prescribed protocols.
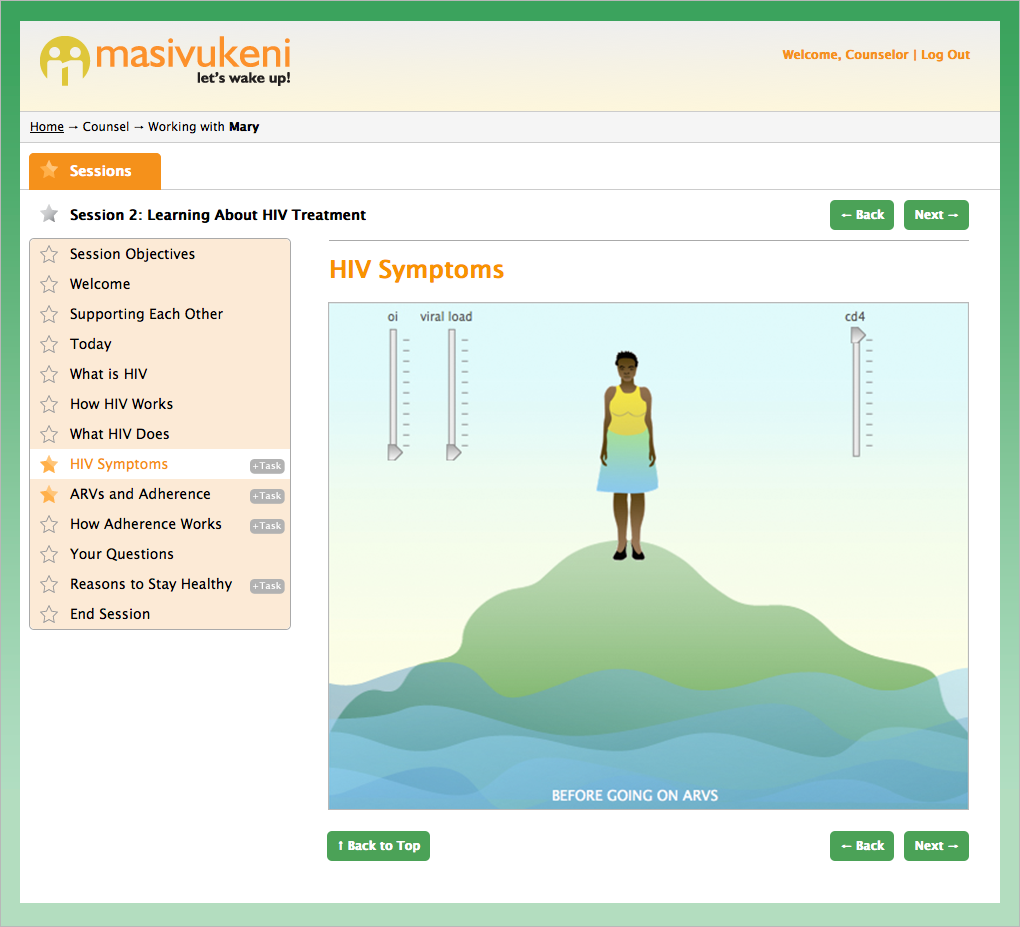
Island Activity: Before ARV's
The "Island Activity" depicts the improvement or decline of a patient's health using a controllable animation of a person on an island surrounded by rising or lowering water, a metaphor which was developed with partners at the pilot clinic. Prior to starting ARV therapy, patients have no control over the water level, which rises with their viral load and opportunistic infections, or over the height of the island, which lowers with their CD4 count (a measure of immune system strength).
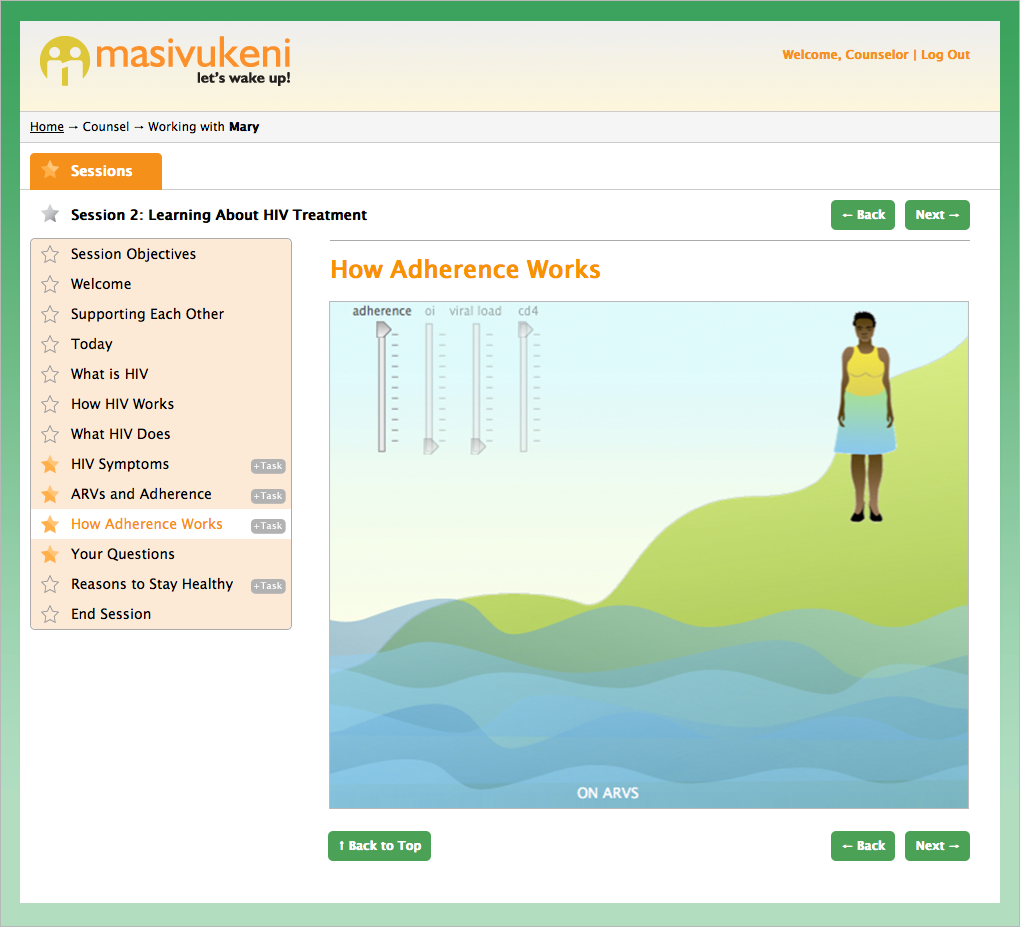
Island Activity: After ARV's
Patients taking ARV's are depicted on a mountain, rather than an island, indicating agency in their ability to manage the illness through adherence to their prescribed medication regimen.
Previous iterations of this activity used scales or other metaphors in which the person themselves and their viral load were in some way separated. Through user research, we realized that it was essential that both our imagery and any metaphors used allow people to see that self, immune system, and virus are wholly connected. Following on this learning, figures shown in the Island Activity are gender-appropriate to the patient, further helping to create a personal connection to the information.
Social Support Activity
During the first session of Masivukeni, a counselor helps the patient identify appropriate supports in their social network and asks the patient to choose a partner to bring to the Masivukeni sessions.
Again, the tree metaphor for this activity developed over time and through extensive work with local communities. Previous iterations were significantly more complex and placed the patient at the physical center of both their community and the activity. Partners at the University of Cape Town helped us to understand that this was a mismatch for the South African mental model of family, in which self and family are organically one and the same. We also came to see that disclosure of HIV-status to the treatment partner was the single most important part of this activity, so more detailed conversation about types of support and problem solving was moved later in the intervention.
Problem Solving Activity
Since many barriers to adherence are practical or logistical in nature, sisters (nurses) with whom we worked suggested practicing problem solving using the actual barriers faced by individual patients. This activity allows patients to "flag" all of the barriers that apply to them, then focus on solving the most pressing or difficult challenge with their counselor.
As we developed this activity, we found that we needed to break the tasks down into much smaller steps than anticipated — as well as simplify on-screen affordances such as buttons and calls to action — in order to address limited literacy and computer experience among users.